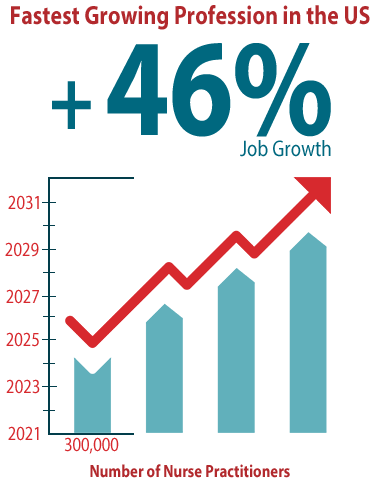
In the United States, nurse practitioners (NPs) are the fastest growing profession in the United States, and according to the Bureau of Labor Statistics (BLS), the number of NPs is expected to grow by 46% over the next 10 years.1 NPs hold a bachelor of science in nursing, complete an NP-focused graduate master’s or doctoral nursing program, and pass a national NP board certification exam. They can practice independently in many states, and can order labs and diagnostic tests, prescribe medications, and help manage the chronic diseases of their patients.
While NPs are needed now more than ever, a new 3-year study showed that NPs have worse outcomes that result in higher costs than that found with emergency department (ED) physicians.2 There appears to be a knowledge gap between NPs and physicians, yet many pharmaceutical and biotech commercial teams do not have a strategy designed to support the particular continuing education needs of NPs. It is critical we pay attention to this group of practitioners when developing educational programs.
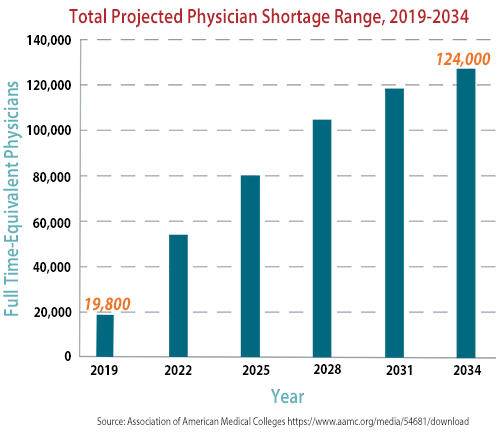
NPs are in high demand, and will continue to be according to current BLS projections. Due to increasing costs, healthcare facilities have grown to rely on providers other than physicians. Payers are looking for ways to lower their healthcare spending costs, and NP salaries, on average, are about half that of physicians. Physician shortages continue to be an issue and will account for a loss of up to 124,000 physicians over the next 10 years.3 Many physicians have gone on to pursue certain specialties, therefore, NPs have stepped in to fill many primary care roles that had traditionally been handled by physicians. The facts are clear—NPs are needed, as well as physician associates (PAs, formerly called physician assistants).
While most of us in the healthcare industry agree that NPs and PAs are critical in providing medical care for patients, it’s important to look at the findings of a comparative study between NPs and physicians that was carried out within the Veterans Health Administration. According to the National Bureau of Economic Research, NPs delivering emergency care without physician supervision and/or collaboration increased lengths of hospital stays for patients by 11%, and raised 30-day preventable hospitalizations by 20% compared with that of physicians in the ED.2
Researchers used a sample of 1.1 million ED visits occurring between January 2017 and January 2020 of patients arriving during similar timeframes and used a quasi-experimental variation in the patient probability of being treated by physicians versus NPs. David Chan, MD, PhD, associate professor of health policy at Stanford University School of Medicine, and Yiqun Chen, PhD, assistant professor of economics at the University of Illinois at Chicago concluded that the higher preventable hospitalization rate “may reflect two possibilities….first NPs have poorer decision making over whom to admit to the hospital, resulting in under admission of patients who should have been admitted and a net increase in return hospitalizations, despite NPs using longer lengths of stay to evaluate patients’ need for hospital admission.”2,4
The other possibility they described was that “NPs produce lower quality of care conditional on admitting decisions, despite spending more resources on treating the patient (as measured by costs of the ED care). Both possibilities imply lower skill of NPs relative to physicians.”2,4
The Association of American Medical Colleges projects that, by 2034, the US will not have enough physicians to treat the number of patients that will need care,3 therefore, NPs will play a critical role and they must be prepared. Now is the time to figure out how best to develop their skills.
What can we do in biopharma to improve the education of NPs?
To answer this question, first, conduct a KOL Identification study of NPs and PAs in your therapeutic area to ensure that those you are utilizing are viewed as credentialed and considered influencers based on their extensive background. A recent study found the physician–NP gap on cost and quality grew with patient complexity, with NPs being more likely to admit patients to the hospital with complex or severe conditions, and lengths of stay and medical costs also rose with the complexity of the patient’s condition.3 Therefore, curriculum for NPs should be more robust for disease states that are more complex.
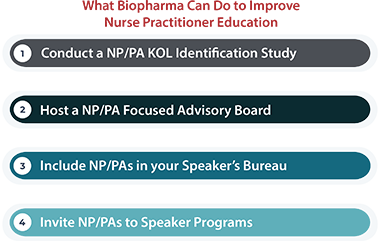
Second, meet NPs/PAs where they are, which means first truly hearing from them in an advisory board setting. Advisory boards focused on NPs and PAs have been drivers to help understand the gaps in knowledge and can create initiatives that help them get up to speed as it relates to their role as practitioners.
Third, ensure that you have included NPs and PAs in your speaker’s bureau. Recognize that when it comes to education, their role is best served speaking to their peers, or on a panel with other scientists and clinicians, when they’ve had significant therapeutic experience. NPs are often preferred by patients as studies demonstrate that NPs connect with patients on a human level and provide excellent compassion.5 So, the work in training this group is less on bedside manner and more on decision making; less on social interaction and more on process.
Finally, have your sales representatives and medical science liaisons spend time with NPs and PAs if your disease state is not complex and they care for those patient types. Invite them to speaker programs within therapeutic areas that they manage. Since they are often hungry for knowledge, a little time spent can go a long way toward improving patient care for these professions that our society needs to help fill our country’s medical needs.
References
- U.S. Bureau of Labor Statistics. Fastest growing occupations: 20 occupations with the highest projected percent change of employment between 2021-3
https://www.bls.gov/ooh/fastest-growing.htm. Accessed February 21, 2023. - Chan DC Jr, Chen Y, for the National Bureau of Economic Research. The productivity of professions: evidence from the emergency department. October 2022
https://www.nber.org/papers/w30608. Accessed February 21, 2023. - Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2019 to 2034.
https://www.aamc.org/media/54681/download. Accessed February 21, 202 - DePeau-Wilson M. Study adds fuel to debate over nurse practitioners’ scope of practice.
https://www.medpagetoday.com/special-reports/exclusives/102289. Accessed February 21, 2022. - Harrison W. Consumers receptive to NP, PA care models. Clinical Advisor.
https://www.clinicaladvisor.com/home/web-exclusives/consumers-receptive-to-np-pa-care-models/. Accessed February 22, 2023.