While clinical excellence is the ultimate driver of positive outcomes, compassion can add significant value to those outcomes in measurable ways. What is compassion? Most scientists agree that compassion is the emotional response to another’s pain or suffering, involving an authentic desire to help. Compassion is included in the American Medical Association’s Principles of Medical Ethics, “A physician shall be dedicated to providing competent medical care with compassion.”1
Recently, I participated in a series of virtual patient advisory boards and, during these meetings, we heard stark insights about how difficult it has been for some patients to get diagnosed and treated for certain rare diseases. We listened intently as we heard from many patients that had gone through years of frustration seeing more than 15 health care providers (HCPs) before they were properly diagnosed and received meaningful treatment.
Several patients stated that along their journey, many HCPs brushed off clear metabolic signs as simply psychological. Ultimately, they did find physicians who were able to help them, but along the way, these were the lucky ones. However, they did not receive the compassionate care that they were seeking.
This made me wonder: How many patients in general give up and are never properly diagnosed, or don’t comply with treatment because they don’t feel a sense of compassion from their HCPs? How many patients stop their treatment?
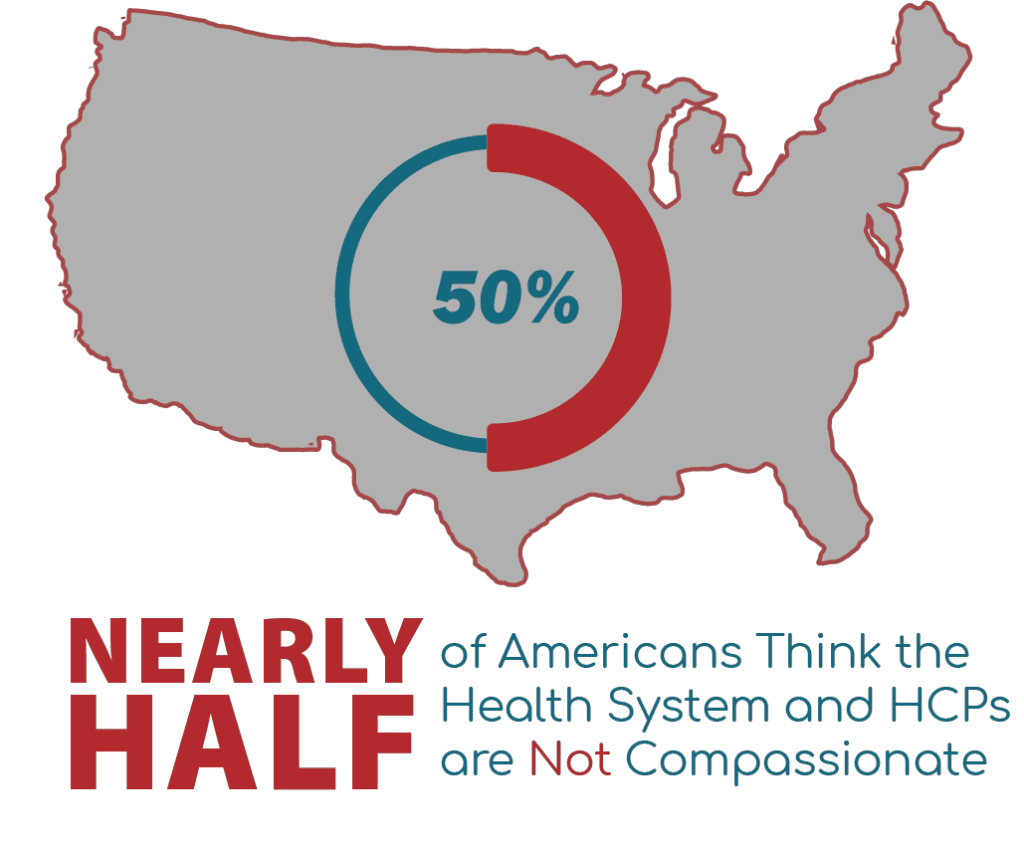
In one study from Harvard Medical School, researchers asked 1300 patients and physicians the question, “Is the U.S. health care system compassionate?” The answer—nearly half of Americans believe that the US health care system and HCPs are not compassionate. Nearly half of the patients noted that it’s not just the system that’s the problem, they indicated that the providers within the health care system are not compassionate.2
Research also shows that physicians routinely miss emotional cues from their patients. In a follow-up study, researchers found that 63% of HCPs said that they have observed a decline in compassionate care over the past 5 years. Researchers studied doctors’ emotional intelligence to understand the associations between emotional intelligence, patient trust, and the doctor-patient relationship. They learned that how the doctors self-rated on emotional intelligence didn’t correlate with how their patients viewed them. Physicians actually miss 60% to 90% of opportunities to respond to patients with compassion.3

“Don’t treat patients as a disease, treat them as a person. When patients feel that you have their best interests at heart, when you have compassion for them, they will do anything you ask them to—and that improves health. It’s a very powerful thing.“
– Michael AbouAssaly, MD – Great River Medical Center, Burlington, IA
Patients feel that they receive less compassion; however, exhausted and burned-out physicians believe that they are only able to provide limited compassionate care due to the current system. It seems that we have a compassion crisis in medicine.
Not only is exhibiting compassion morally the right thing to do, but studies demonstrate that compassion heals. It calms physiological response to stress, improves the autonomic nervous system, and increases oxytocin, known as the “trust” or “love” hormone. Respiratory rates decline, heart rates decrease, heart rate variability increases, and blood pressure lowers.

A University of Colorado study—supported by a research grant from the National Institutes of Health—demonstrated that in 85% of the outcomes measured across 34 controlled experimental studies of patients recovering from a heart attack or surgery, there was a positive association between the psychological and emotional support received from HCPs that resulted in favorable clinical outcomes. They concluded that psychological and emotional support was associated with an improvement in patient recovery.4
Therefore, compassion matters.
In my own experience in health care education over the past 30 years, I can recall physicians sharing that the invention of new, highly effective treatments has allowed them to spend less time with their patients. As I’ve worked in dozens of therapeutic areas, I hypothesize that compassion increases significantly where there are very few tools for doctors to prescribe for the patient—like pharmacological, biological, nutritional, or medical devices. When physicians have a wealth of available tools, they tend to rely on the data and tools to carry the clinical excellence forward. When the tools are unavailable for patient care, they must rely on compassion in conjunction with any other clinical excellence they can muster.
Mike AbouAssaly, MD, named Family Physician of the Year in the state of Iowa as well as a top 5 finalist for Physician of the Year by the American Association of Family Practitioners, has built a world-class obesity center in Burlington, IA. Dr. AbouAssaly explained, “Medical students are trained to focus on disease states and treatment of disease, but weren’t taught about including compassion in conditions like obesity. Early in my career, I had taken for granted that patients knew how to live a healthy lifestyle. I thought every patient knew how to lose weight. I would send them off to go and lose 35 pounds, but then they’d come back in 6 months and nothing changed. I learned that my patients needed to be taken by the hand to address their life’s timeline; we go back to their history, their family life, their story, and with compassion, help them get to the core of what’s causing their condition.”

Dr. AbouAssaly continued to describe the passion he has for his patients, “The stigma of obesity is real; nobody wakes up wanting to be heavy. They’re embarrassed because they blame themselves. I help my patients understand what it takes to get a healthy lifestyle back. Just a subtle 5% to 7% weight loss makes a dramatic impact, so we set realistic goals. We start there and take it week-by-week, month-by-month. We meet the patient where they are by modifying the diet that they already know. We see them as a person, not as an obese person. When we take the time to do this with patients, they know that you care because you took the time to learn about them as a person.”
As a result of these efforts, 87% of his patients reach the 15% weight loss goal in 6 months, and 92% reach the goal after 12 months.
This is where we in the pharmaceutical and biotech space can have an impact.
While highly effective, we are only beginning to realize how to use compassionate care for patients. Studies have existed for a long time that prove how many conditions can be clinically improved with compassionate care. For example:
- Compassion significantly reduced pain in irritable bowel syndrome5
- Among patients with diabetes, the odds of optimal blood sugar control were 80% higher with highly compassionate physicians6
- Patients with breast cancer had significantly higher adherence to tamoxifen 4 years after their cancer diagnosis when they perceived receiving “the right amount” of emotional support7
So what are those things we can do to improve clinical excellence for doctors and patients with your pharmaceutical marketing strategies and your pharmaceutical education? Consider these ideas:
- Coach your speakers to encourage clinicians to spend 40 seconds displaying compassion and actively listening to patient concerns. The median amount of time before a doctor typically interrupts a patient when they’re discussing their chief complaint is 11 seconds. Extending the time up to 40 seconds of expressed compassion tends to help patients feel heard and that the doctor cares.8
- Build tools and training around physicians to ensure that they make eye contact with the patient. For example, when physicians are talking about treatment, and they’re busy looking at a computer screen, patients feel disconnected and are less likely to follow the orders when they don’t feel like they are being focused on.
- Teach speakers why tone of voice and mimicking patient expressions help patients feel valued, appreciated, and connected.
- Ask Advisory Board meeting participants how they believe compassionate care influences the treatment paradigm for patients within the disease state and your brand.
- Remember that medicine is always for the patient. When communicating to physicians, remind them that compassion improves treatment adherence. Again, remind them that listening to their patients for 40 seconds up front will likely improve treatment compliance.
- Sales representatives can encourage compassion. Compassion is contagious; commend office staff when you see them offer support and empathy to patients as soon as they enter the front door.
Dr. AbouAssaly believes that active listening matters. “Don’t treat patients as a disease, treat them as a person. When patients feel that you have their best interests at heart, when you have compassion for them, they will do anything you ask them to—and that improves health. It’s a very powerful thing.”
Compassion matters. In health care—just as in life—people caring for people make the world a better place. With evidence so strong, it’s time for us to harness both our rigorous scientific process and the art that kindness, respect, and love, do, in fact, heal.
1American Medical Association. AMA principals of medical ethics. Accessed June 20, 2023.